Arthritis is a very common disease, however it is not entirely understood by the general masses. Actually, “arthritis” is not a single disease; it is an informal way of referring to joint pain or joint disease. Arthritis is an inflammation of the joints. It can affect one joint or multiple joints.
One of the most common misconceptions is that most people think of arthritis as a condition that strikes older people. In fact, different types of arthritis affect people of all ages.
There are more than 100 different types of arthritis and related conditions. People of all ages, sexes and races can and do have arthritis, and it is the leading cause of disability in America. More than 50 million adults and 300,000 children have some type of arthritis. It is most prevalent among women and occurs more frequently as people get older.
But arthritis is not a new phenomenon; it has afflicted mankind for hundreds of years. There’s evidence in centuries-old skeletal remains of arthritic joints, says Rochelle Rosian, MD, a Cleveland Clinic rheumatologist in Solon, Ohio.
“Over the past 100 years, there’s a lot more knowledge of the science of the musculoskeletal condition and the immune system,” says Dr. Rosian. Researchers have identified more than 100 various types of arthritis, and counting. Many inflammatory conditions accompanied by fevers and immune dysfunction are now understood to be conditions related to arthritis, and more conditions are introduced to this list all the time. Some types of arthritis also affect the heart, eyes, lungs, kidneys and skin as well as the joints.
Arthritis Causes, Symptoms and Types
Cartilage is a firm but flexible connective tissue in your joints. It protects the joints by absorbing the pressure and shock created when you move and put stress on them. A drop in the normal amount of this cartilage tissue can cause some forms of arthritis.
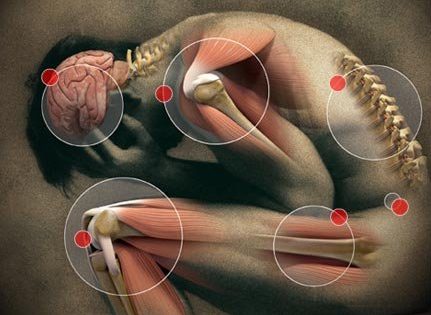
Common arthritis joint symptoms include swelling, pain, stiffness and decreased range of motion. Symptoms may come and go. They can be mild, moderate or severe. They may stay about the same for years, but may develop or get worse over time.
But arthritis appears in different forms, and the causes of arthritis vary by type. Joint pain, stiffness, and swelling are the most common symptoms of arthritis. Your range of motion may also decrease, and you may experience redness of the skin around the joint.
Many people with arthritis notice their symptoms are worst in the morning. Severe arthritis can result in chronic pain, inability to do daily activities and make it difficult to walk or climb stairs.
Arthritis can cause permanent joint changes. These changes may be visible, such as knobby finger joints, but often the damage can only be seen on X-ray.
The symptoms of arthritis usually develop over time, but they may also appear suddenly. Arthritis is most commonly seen in adults over the age of 65, but it can also develop in children, teens, and younger adults. Arthritis is more common in those individuals who are overweight. In addition, arthritis inflammation can result from a variety of conditions and diseases, like gout, lupus, and fibromyalgia.
There are different types and causes of arthritis:
- Osteoarthritis (OA). Normal wear and tear causes OA, also called degenerative joint disease, the most common and most frequently diagnosed form of arthritis. An infection or injury to the joints can exacerbate this natural breakdown of cartilage tissue.
Your risk of developing OA may be higher if you have a family history of the disease. Osteoarthritis occurs when the cartilage inside a joint disintegrates. When the cartilage – the slick, cushioning surface on the ends of bones – wears away, bone rubs against bone, causing pain, swelling and stiffness. Over time, joints can lose strength and pain may become chronic. Risk factors include excess weight, family history, age and previous injury (an anterior cruciate ligament, or ACL, tear, for example). If joint symptoms are severe, causing limited mobility and affecting quality of life, some of the above management strategies may be helpful, but joint replacement may be necessary. Osteoarthritis can prevented by staying active, maintaining a healthy weight, and avoiding injury and repetitive movements. This form of arthritis most commonly affects the knees, hips, low back, neck, and hands, and most often occurs after the age of 40.
- Rheumatoid arthritis (RA). This type of arthritis occurs when the lining inside joints becomes inflamed and irritated, causing joint damage and pain. It most often occurs in small joints in the wrists, fingers, and hands.
RA is an autoimmune disease that usually strikes between the ages of 30 and 50. Women are most often affected, though children may also develop RA.
RA is an autoimmune disorder. It occurs when your body’s immune system attacks the tissues of the body. These attacks affect the synovium, a soft tissue in your joints that produces a fluid that nourishes the cartilage and lubricates the joints. RA is a disease of the synovium that will invade and destroy a joint. It can eventually lead to the destruction of both bone and cartilage inside the joint.
A healthy immune system is protective. It generates internal inflammation to get rid of infection and prevent disease. But the immune system can go awry, mistakenly attacking the joints with uncontrolled inflammation, potentially causing joint erosion and may damage internal organs, eyes and other parts of the body. The exact cause of the immune system’s attacks is unknown, but scientists have discovered genetic markers that increase your risk of developing RA tenfold.
Sign Up For Our FREE Inner Circle Membership & Receive Exclusive Natural Health Information
Rheumatoid arthritis and psoriatic arthritis are examples of inflammatory arthritis. Researchers believe that a combination of genetics and environmental factors can trigger autoimmunity. Smoking is an example of an environmental risk factor that can trigger rheumatoid arthritis in people with certain genes. In the case of RA, there are certain additional symptoms that might occur: you may feel tired or experience a loss of appetite due to the inflammation that immune system activity causes. You may also become anemic - meaning your red blood cell count decreases - or have a slight fever. Severe RA can cause joint deformity if left untreated.
- Infectious Arthritis. A bacterium, virus or fungus can enter the joint and trigger inflammation.
Examples of organisms that can infect joints are salmonella and shigella (food poisoning or contamination), chlamydia and gonorrhea (sexually transmitted diseases) and hepatitis C (a blood-to-blood infection, often through shared needles or transfusions). In many cases, timely treatment with antibiotics may clear the joint infection, but sometimes the arthritis becomes chronic.
- Metabolic Arthritis. Uric acid is formed as the body breaks down purines, a substance found in human cells and in many foods.
Some people have high levels of uric acid because they naturally produce more than is needed or the body can’t get rid of the uric acid quickly enough. In some people the uric acid builds up and forms needle-like crystals in the joint, resulting in sudden spikes of extreme joint pain, or a gout attack. Gout can come and go in episodes or, if uric acid levels aren’t reduced, it can become chronic, causing ongoing pain and disability.
- Juvenile arthritis (JA). This includes any type of arthritis that strikes children younger than age 18.
What causes arthritis to develop at such an early age is unknown, but it occurs more often in girls than boys. JA typically strikes the ankles, knees, and wrists, and may also affect the hips, neck, jaw, and shoulders. There are many types of juvenile arthritis, the most common being juvenile rheumatoid arthritis, or JRA. There are three specific forms or juvenile rheumatoid arthritis: polyarticular (many joints) JRA, pauciarticular (four or fewer joints), and systemic onset (affecting the whole body).
How Is Arthritis Diagnosed?
Diagnosis of arthritis will start with your doctor performing a physical exam. During the exam, your doctor will check for fluid around the joints, warm or red joints, and limited range of motion in the joints.
Extracting and analyzing inflammation levels in your blood (rheumatoid factor test) and joint fluids can help your doctor determine what kind of arthritis you have. A rheumatoid factor test looks for an antibody called a rheumatoid factor. About 80% of people with RA eventually have this antibody, although it’s possible to have the rheumatoid factor in your blood and not have RA.
Another test measures your erythrocyte sedimentation rate. People with RA tend to have abnormally high sedimentation rates.
Doctors commonly use imaging scans such as X-ray, MRI, and CT scans to produce an image of your bones and cartilage. This is so they can rule out other causes of your symptoms, such as bone spurs.
What official medicine offers for Arthritis Treatment?
The main goal of treatment is to reduce the amount of pain you’re experiencing and prevent additional damage to the joints. Improving your joint function is also important. Your doctor may prescribe you a combination of treatment methods to achieve the best results.
Medication
A number of different types of medication treat arthritis. They include:
- analgesics, e.g., hydrocodone (Vicodin) or acetaminophen (Tylenol): effective for pain management, but don’t help decrease inflammation.
- nonsteroidal anti-inflammatory drugs (NSAIDs), e.g., ibuprofen: help control pain and inflammation
- menthol or capsaicin creams: block the transmission of pain signals from your joints
If you have RA, your doctor may put you on corticosteroids or disease-modifying antirheumatic drugs (DMARDs), which suppress your immune system.
Surgery
Surgery to replace your joint with an artificial one may be an option. This form of surgery is most commonly performed to replace hips and knees.
If your arthritis is most severe in your fingers or wrists, your doctor may perform a joint fusion. In this procedure, the ends of your bones are locked together until they heal and become one.
Physical Therapy
Physical therapy involving exercises that help strengthen the muscles around the affected joint is a core component of arthritis treatment.
They say that there is no cure for arthritis and the right treatment can only reduce the symptoms.
Sources & References
- (2012, April 12). Centers for Disease Control and Prevention. Retrieved April 16, 2012, from http://www.cdc.gov/chronicdisease/resources/publications/aag/arthritis.htm
- http://www.everydayhealth.com/arthritis/index.aspx
- (2011, January 22). Mayo Clinic.Retrieved April 16, 2012, from http://www.mayoclinic.com/health/arthritis/DS01122
- (2012, February 2). National Center for Biotechnology Information.Retrieved April 16, 2012, from http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0002223/
- What is Osteoarthritis? (n.d.). Arthritis Foundation.Retrieved April 16, 2012, from http://www.arthritis.org/what-is-osteoarthritis.php
- What is Rheumatoid Arthritis? (n.d.). Arthritis Foundation.Retrieved April 16, 2012, from http://www.arthritis.org/types-what-is-rheumatoid-arthritis.php
- (2012, February 2). Retrieved from http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0002223/
- (2015, July 22). Retrieved from http://www.cdc.gov/chronicdisease/resources/publications/aag/arthritis.htm
- Mayo Clinic Staff. (2014, July 15). Arthritis. Retrieved from http://www.mayoclinic.com/health/arthritis/DS01122
- Rheumatoid arthritis causes. (n.d.). Retrieved from http://www.arthritis.org/about-arthritis/types/rheumatoid-arthritis/causes.php
- Understanding arthritis. (n.d.). Retrieved from http://www.arthritis.org/about-arthritis/understanding-arthritis/